A dynamic team with an ambitious remit reflects on the story so far
Archives: Recovery Stories
Mosaic on course for 2014
Exciting educational links are being made at the Living Well Partnership site
Vital link to personal budgets
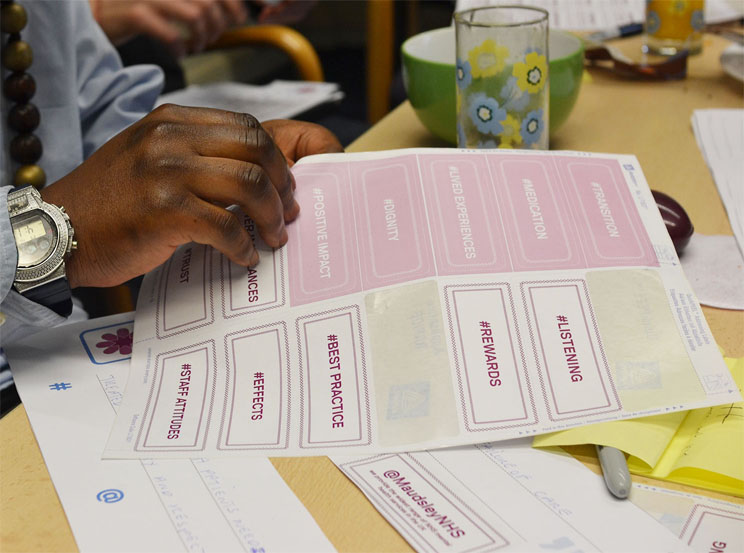
A new report and toolkit have been shaped by the work of two local lived experience advisors
Who cares?
It’s not just those who use services who appreciate peer support, carers also need someone to talk to
From just about surviving to thriving
An evaluation of peer projects has produced compelling evidence for shaping the future
The missing link
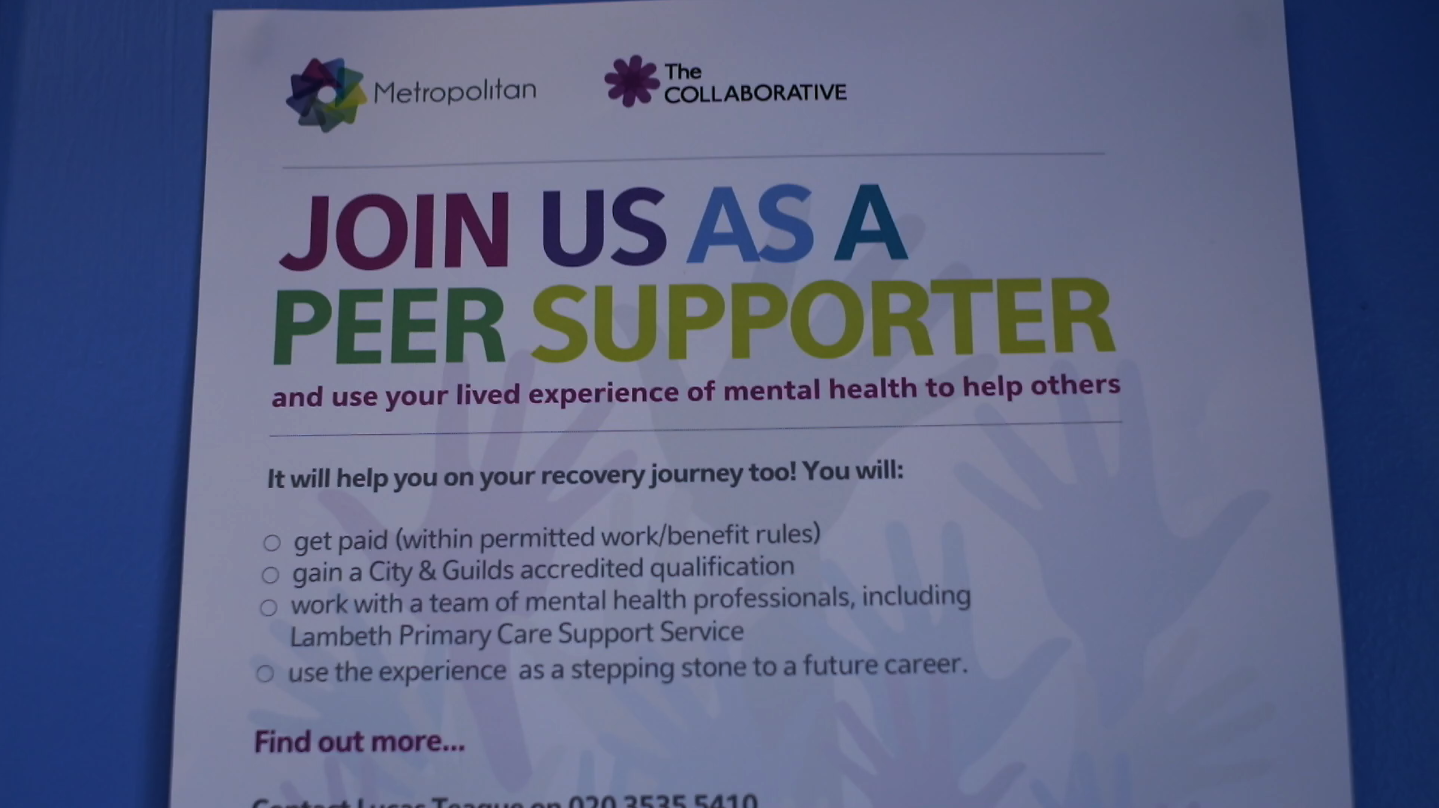
Lucas Teague explains what it takes to be Co-ordinator of a successful peer support service