The North Lambeth Network Hub opened on 18 November 2013. It was born out of a desire from the Lambeth Collaborative to improve outcomes for service users and to grow an integrated structure of support for people in primary care.
The Hub is comprised of:
- A nurse, occupational therapist, social worker, two psychiatrists from the South London and Maudsley NHS Foundation Trust (SLaM) and Lambeth Council,
- The Primary Care Support Service (PASS) , a group of nurses working with Clapham Family Practice in GP surgeries,
- The Community Options Team (COT), a team of voluntary sector providers across Mosaic, Look Ahead, Penrose, Certitude and Thames Reach, together with
- A growing peer support service hosted by Certitude.
Its aim is to work within a ‘primary and social model’ of support and work co-productively with service users and carers to support them to recover and stay well, be able to make their own choices and participate in their communities.
Working co-productively means:
- Recognising people as assets – recognising that people are resourceful and can use their strengths and skills to support their own recovery
- Building on people’s existing capabilities – supporting people to identify their skills and how to use them to meet their goals
- Peer support networks – working with service users to foster supportive relations between themselves
- Blurring distinctions – thinking creatively, not always using services in their traditional sense
- Facilitating rather than delivering – supporting people to recover rather than ‘doing to and for’ people
- Mutuality and reciprocity – thinking about how people and organisations can ‘trade’ skills or resources to support each other.
Together we are the new front door to mental health services in North Lambeth as we have replaced the community mental health team function of deciding who would benefit from secondary care intervention and we are beginning to work with people being discharged from SLaM back to their GP.
We are still developing the service but can now report on our initial six month activity.
Main aims
Our main aims are:
- To reduce inappropriate referrals to SLaM
- To reduce the number of people being supported by the Mood and Anxiety Community Mental Health Team in SLaM (the team that used to be the entry point to support from the community mental health teams) by 10%
- To offer alternative support to 400 people so that they can be supported by their GP and not need to be referred to SLaM. We also wish to help a wider population where we can intervene earlier and hence reduce escalation of crises.
We also want to address GP concerns as they have reported issues of:
- There being ‘too high thresholds to access support’ which means that GPs feel that they have to wait for people’s health to deteriorate before services will offer support
- Not knowing how to access general mental health advice
- Not knowing how to access social support for their patients
We offer people up to 12 weeks of ‘re-ablement’ support. This means offering focused, goal orientated support together with a wider Network of services to support people to learn or reconnect with their skills to foster their recovery.
Initial results
People being introduced to the Hub
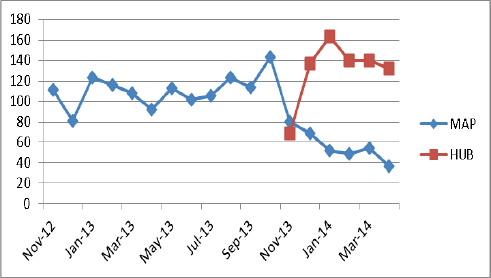
The Hub has received 781 introductions since opening. The red line shows when we opened (18th November) and shows the numbers of introductions we received, and the blue line shows the numbers received by the community mental health team. Onward referral to SLaM has reduced significantly.
Figure One: Numbers of referrals received by the Community Mental Health Team (CMHT) and numbers introduced to the Hub.
Most service users are not known to SLaM or other mental health services or Accident & Emergency Departments. Most are introduced by the GP and 40% (309) of people who were introduced were offered alternative support via the Hub.
What support are people receiving when they are introduced?
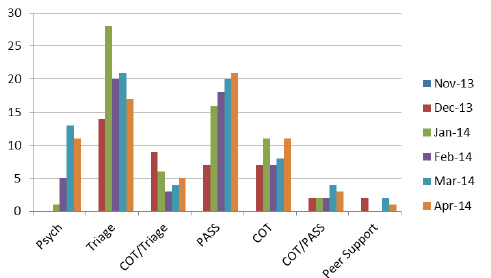
One of the key strengths of the Hub is that people can receive the help that they need from the outset, for example if someone requires a medical assessment, or support with their medication, and also has issues with their housing and benefits; teams can work with the person immediately. The chart below shows the numbers of people who were helped by the different teams.
Figure Two: Numbers of people who were supported by the Hub
Service user views
We now have a service user feedback form, but to get some early results we asked 5 peer supporters to contact 60 people to ask them about how they found the service. They were able to talk to 17 people.
In all:
– 70% felt their goals were ‘definitely met’ or ‘met to some extent’
– 15 out of the 17 identified being ‘involved in how their goals were met’
– Only one person stated they did not discuss how to get help in an emergency
– The majority of people reported their experience as ‘excellent’ or ‘good’.
Improvements suggested centred around wanting more than 12 weeks of support, wanting more information about what was on offer, and the need to improve the waiting area.
GP Views
Similarly, we asked GPs what they felt about the service. We received 10 responses from 6 surgeries. The following was found;
- 60% of GPs reported an understanding of what happened in the Hub, 40% ‘to some extent’
- 50% reported finding the introduction process, ‘easy’, 30% ‘satisfactory’, and 20% ‘difficult’
- 70% stated they received feedback, 30% sometimes
Other comments included:
‘It is much better than the previous CMHT’. It really seems to be better organised than it used to be ‘Thank you’.
Suggestions centred around how we communicate the different services to users so that they are not confused, giving the GP a key contact name of the person supporting the service user and a suggestion of how the Hub can support people on discharge from SLaM.
One GP was concerned that people ‘are still getting bounced around the system’ meaning that sometimes people are referred to lots of teams before they receive help.
What next?
We have lots to do, but our priorities are:
1. Thinking about how we work in a more co-productive way. We want to:
- Design an Introduction Form. This form can be given to users before they see one of the Hub staff so that they can think through what and how they can be supported. We want to make sure that we are working with peoples’ priorities rather than service priorities and we think that by guiding people through what they may like to say will promote this.
- Pilot a MY Wellbeing Pack: This pack will be given to people when they come to the Hub and will summarise all the key pieces of information, such as medication, side effects, what needs doing next, key contact points in case future help is needed. We want everyone to know about peer support services such as Solidarity in a Crisis, which supports people at times of crises on the phone seven nights a week and in the community at the weekend.
- Begin hosting a monthly open event at the Living Well Partnership, so that everyone, service users, staff, carers, members of the public can get to know all the services in the Network and the many opportunities open to them. Services include employment, training, workshops discussing mental health, support plans, services offering practical support, information.
- At a later date we want to pilot how people can self refer to the service and chose who they see in the Hub.
- Think more about how users and peers can be involved in all aspects of what we do.
2. Roll out a South Hub by December 2014
3. Develop how we are working to support people leaving SLaM.
More information
If you would like to see the full report, or would like further information, please contact Sue Field, at S.Field2@nhs.net.
Sue Field, Programme Director, Provider Alliance Group (4 August 2014)
For an example about how the Hub has supported people read Matt’s story here
Read Sue Field’s personal story on the journey to the Living Well Hub launch
For more information about the Living Well Network Open Event please click here

